<client>
huckleberry house & can't stop columbus
<team>
Merry Austin, Joshua Forrest, Eugene Karnaoukhov, Joe Owens
<role>
service designer
<deliverables>
findings deck & executive presentation
<challenge>
Discover how telehealth has affected social workers and staff of Huckleberry House whose work with homeless youth has been affected by the pandemic and social unrest.
<approach>
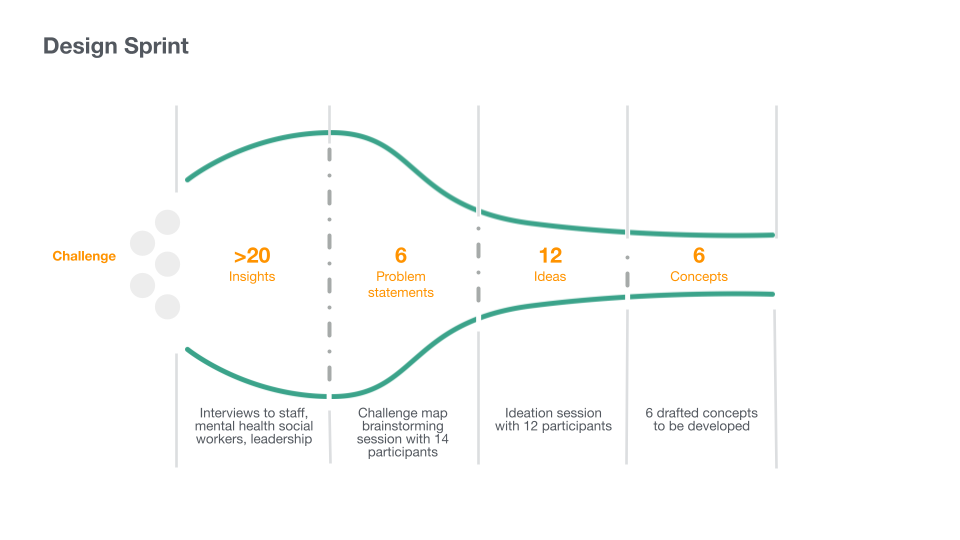
This project piggybacked off the efforts of a previous design sprint in collaboration with a partner of Huckleberry House (Huck House) called Star House & The Columbus Foundation. We refined our insights by conducting a glut of interviews with the therapists and administration at Huck House to uncover what was happening on the frontlines and where specific elements of friction were on the rise.
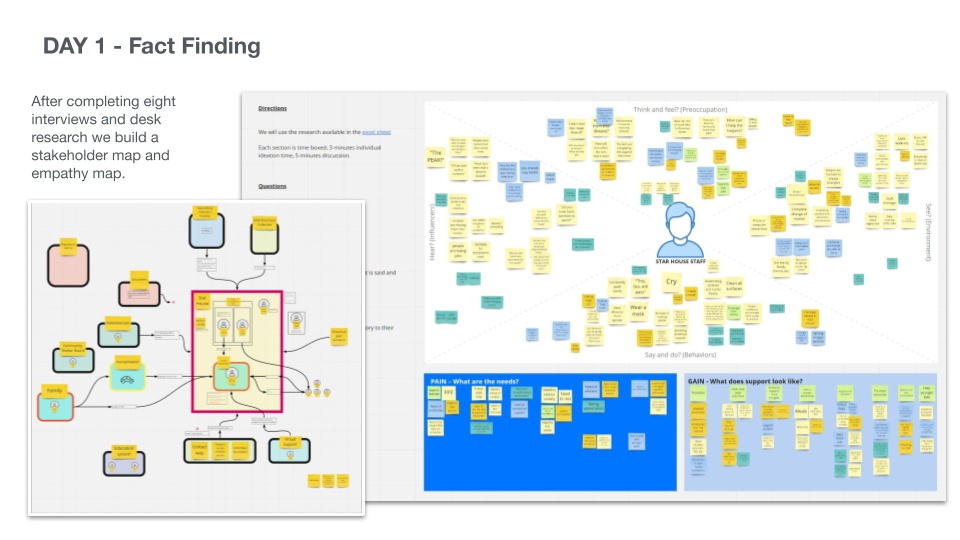
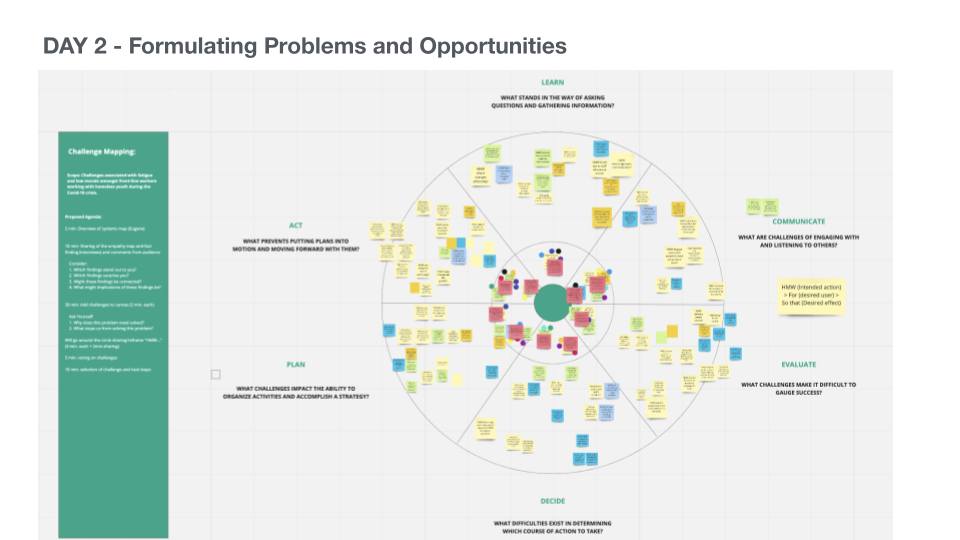
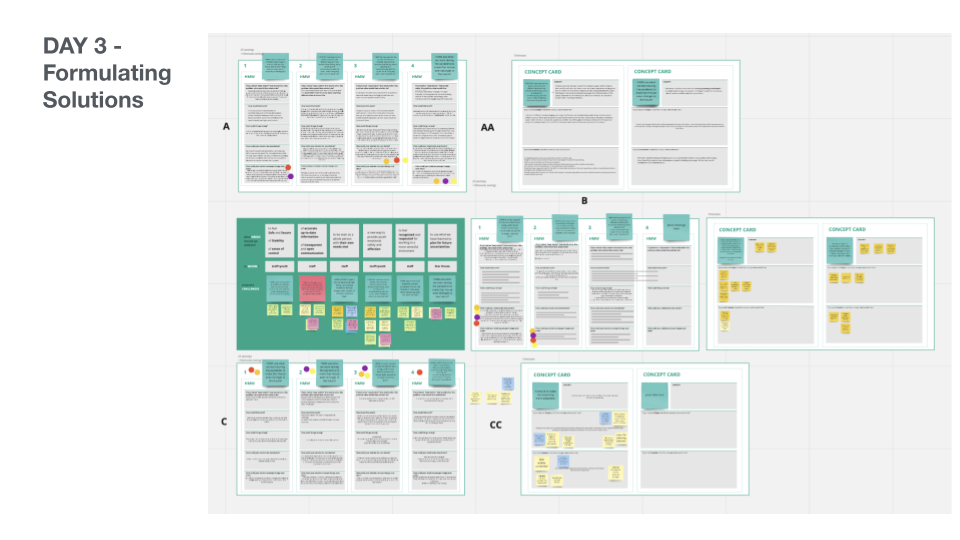
The former effort was collaborative with 3 different co-creation sessions to define the problem with a fact-finding session, formulate the problem and opportunities with a challenge mapping, and then formulate solutions in a round-robin concept card write-up. This set up the foundation of understanding for our work with Huck House. By this point, the first wave of COVID-19 was in full effect and staff were dealing with both the ramifications of the lockdown and many months into the transition into telehealth. These interviews uncovered 3 specific insights that stood out to our team.
The former effort was collaborative with 3 different co-creation sessions to define the problem with a fact-finding session, formulate the problem and opportunities with a challenge mapping, and then formulate solutions in a round-robin concept card write-up. This set up the foundation of understanding for our work with Huck House. By this point, the first wave of COVID-19 was in full effect and staff were dealing with both the ramifications of the lockdown and many months into the transition into telehealth. These interviews uncovered 3 specific insights that stood out to our team.

<key insights>
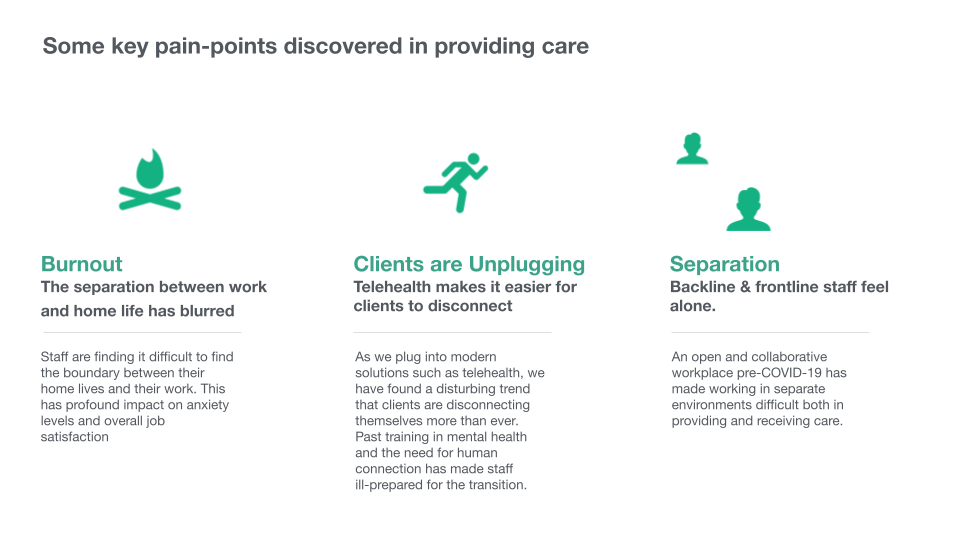
[burnout] the separation between work and home life has blurred
Huckhouse staff is finding it difficult to find the boundary between their home lives and their work. This has a profound impact on anxiety levels and overall job satisfaction
Huckhouse staff is finding it difficult to find the boundary between their home lives and their work. This has a profound impact on anxiety levels and overall job satisfaction
[clients are unplugging] telehealth clients aggressively disconnect
As we plug into modern solutions such as telehealth, there is a disturbing trend that clients are disconnecting themselves more than ever. Past training in mental health and the need for human connection has made staff ill-prepared for the transition
As we plug into modern solutions such as telehealth, there is a disturbing trend that clients are disconnecting themselves more than ever. Past training in mental health and the need for human connection has made staff ill-prepared for the transition
[separation] backing & frontline staff feel alone
An open and collaborative workplace pre-COVID-19 has made working in a separate environment difficult both to provide and receive care
An open and collaborative workplace pre-COVID-19 has made working in a separate environment difficult both to provide and receive care
<outcomes>
It was clear that the transition to telehealth and the shutdown of various government offices (such as BMV/DMVs) was directly affecting the level of care and resolution that staff could give their patients. The frontline staff was experiencing this growing frustration first hand and were making attempts to express this to an increasingly disconnected administration which lead to a sharp divide. This information was put together along with their united strengths in a presentation with the intent of provoking and uniting our clients to rally and move forward together as their best selves.
<some key needs expressed>
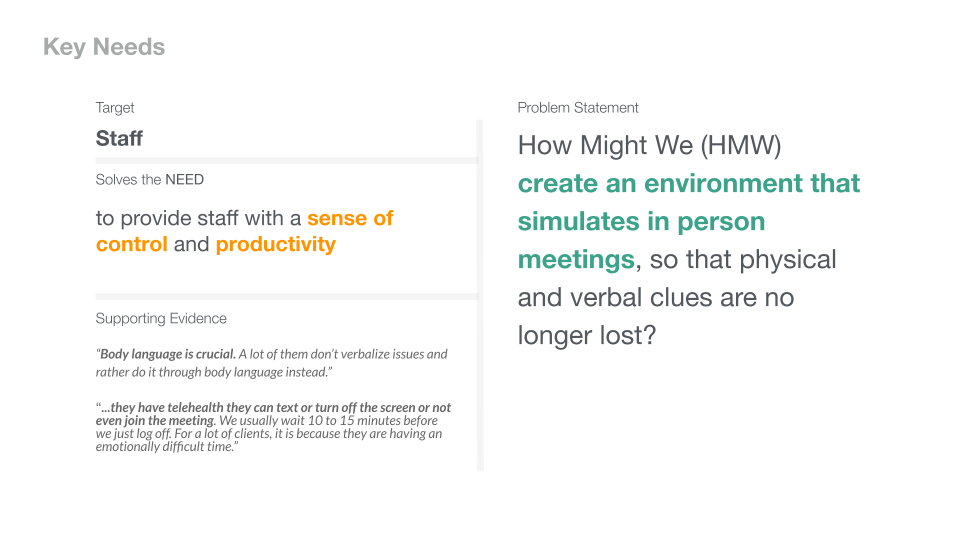
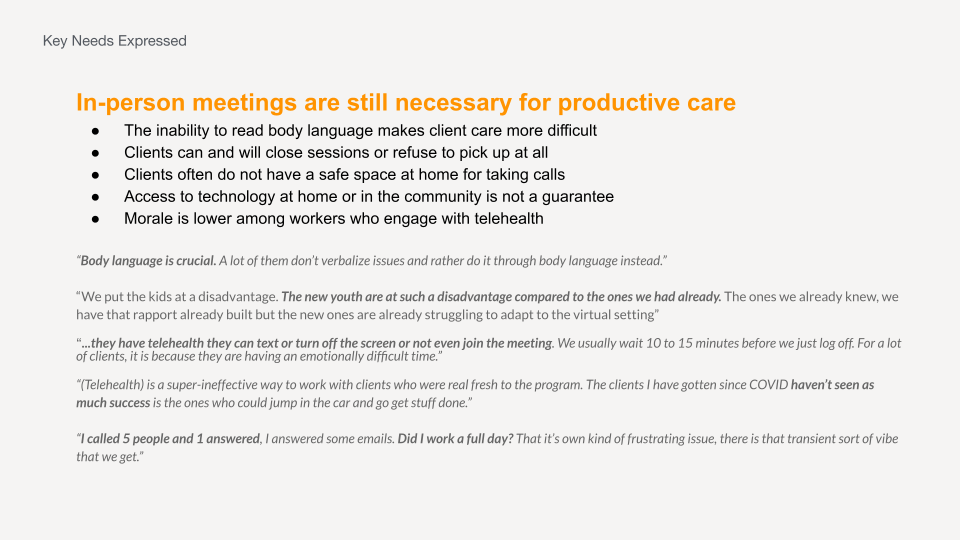
[in-person meetings are still necessary for productive care]
• inability to read body language makes client care more difficult
• clients can and will close sessions or refuse to pick up at all
• clients often do not have a safe space at home for taking calls
• access to technology at home or in the community is not a guarantee
• morale is lower among workers who engage with telehealth
"(telehealth) is a super-ineffective way to work with clients who were real fresh to the program. The clients I have gotten since COVID haven't seen as much success as the ones who could jump in the car and get things done"
[staff are all dealing with different degrees of burnout]
• younger clinical staff members may not be self-aware enough to identify the signs of burnout
• staff feel as though it is hard to gain traction with their clients
• work does not feel a reward nor is it as productive as it was pre-COVID-19
• staff members have increased the number of patients in their care
• clients are suffering anger, trauma, and more due to the current situation with COVID-19
"I have gotten a lot more clients during COVID. I went from 15 clients to 23 to 25. So that's a lot more people to juggle and everyone is furious because they are all unemployed."
[teams feel disconnected from each other]
• there is a distinct gap between direct health, telehealth, and administration
• deep feelings of isolation are being felt among telehealth staff
• staff members are seeking that same sense of unity they had pre-COVID-19
• knowledge gaps between direct care and backline staff make client treatment more difficult
• individual teams are feeling closer to each other than to the greater whole
"Something that is missing right now. That sense of unity and togetherness is really missing. A common mission. We're all on the same page in terms of what we are trying to do."